Comprehensive Guide to Phlebitis: Causes and Treatment for Optimal Vascular Health

Vascular health plays a pivotal role in overall well-being, supporting essential functions such as blood circulation, nutrient delivery, and waste removal. Among the numerous vascular conditions, phlebitis stands out due to its potential to cause discomfort, complicated health issues, and impact on quality of life. Understanding the causes of phlebitis and exploring effective treatment options is crucial for maintaining healthy veins and preventing serious complications.
What Is Phlebitis? An Overview of Vascular Inflammation
Phlebitis, also known as venous inflammation, is a condition characterized by inflammation of a vein. It commonly affects the superficial veins just beneath the skin but can also involve deeper veins, leading to a more serious condition called deep vein thrombosis (DVT). The inflammation results from various factors, which alter the normal structure and function of the affected vessel.
Understanding the distinctions and commonalities between superficial and deep vein phlebitis is essential for accurate diagnosis and management. Both forms require tailored treatment strategies grounded in vascular science and clinical expertise.
Primary Causes of Phlebitis: Unveiling the Underlying Factors
Identifying the underlying causes of phlebitis is fundamental in preventing its occurrence and optimizing treatment. The most common factors include:
1. Trauma and Injury
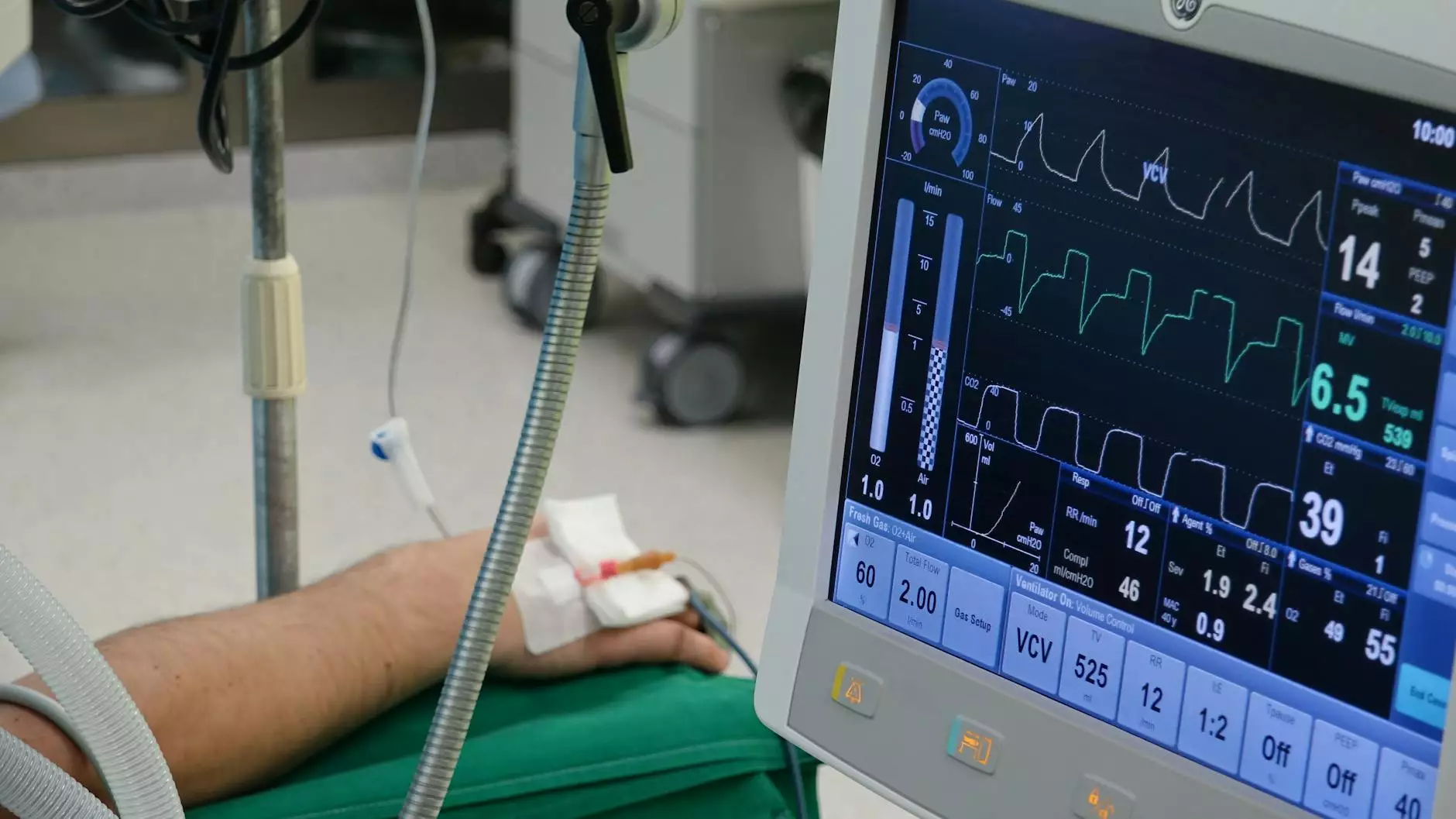
Physical injury, such as blunt trauma, surgical procedures, or intravenous injections, can damage the vessel wall, leading to inflammatory responses. Surgical sites and catheter insertions are particularly susceptible to developing phlebitis when the vein lining is compromised.
2. Prolonged Immobility
Extended periods of inactivity, such as long-haul flights, bed rest, or sedentary lifestyles, impair blood flow through the veins. This stagnation increases the risk of venous inflammation, especially in individuals with pre-existing vascular vulnerabilities.
3. Infections and Skin Conditions
Infections penetrating the skin or surrounding tissues can extend into the veins, causing inflammation. Conditions like cellulitis or skin ulcers may contribute to the development of phlebitis, especially if bacteria invade the vascular system.
4. Blood Clot Formation
Presence of thrombi (blood clots) within veins, such as in deep vein thrombosis, can incite inflammatory reactions. The clot acts as an irritant, damaging the vessel wall and triggering inflammation.
5. Venous Catheters and IV Lines
Medical devices such as intravenous lines can serve as foreign bodies that irritate vein walls, especially if placed improperly or left in situ for extended durations. This mechanical irritation fosters an environment conducive to phlebitis.
6. Varicose Veins and Venous Insufficiency
Chronic venous insufficiency and varicose veins lead to faulty blood flow and vein dilation, heightening susceptibility to inflammation and clot formation.
7. Underlying Medical Conditions
Autoimmune diseases like lupus, certain cancers, or clotting disorders increase the risk of vein inflammation due to systemic vascular involvement.
Recognizing Symptoms of Phlebitis
Early detection of phlebitis relies on recognizing its characteristic symptoms, which often include:
- Redness along the affected vein
- Swelling and warmth in surrounding tissues
- Pain or tenderness, especially when the area is touched or pressure applied
- Hardening or cord-like feeling in the vein
- Discoloration or bluish hue in some cases
If symptoms extend or worsen, especially with signs of systemic illness such as fever or chills, immediate medical attention is warranted to rule out deeper or more dangerous vascular issues.
In-Depth: Phlebitis Causes and Treatment
Understanding the Pathophysiology of Phlebitis
The pathogenesis of phlebitis involves an inflammatory cascade initiated by endothelial injury. Damage to the vein's inner lining exposes subendothelial tissues, activating the immune system and attracting inflammatory cells. This process results in swelling, redness, and pain. When clotting factors are involved, thrombus formation can further complicate the condition, culminating in deep or superficial vein thrombophlebitis.
Effective Treatment Strategies for Phlebitis
Dealing with phlebitis causes and treatment requires a multifaceted approach tailored to the severity and underlying cause:
Conservative Management
- Rest and Elevation: Elevating the affected limb reduces swelling and promotes venous return.
- Compression Therapy: Use of graduated compression stockings supports vein walls and improves blood flow.
- Application of Cold Compresses: Applying ice packs decreases inflammation and alleviates pain.
- NSAIDs: Non-steroidal anti-inflammatory drugs like ibuprofen effectively reduce pain and inflammation.
- Hydration and Mobility: Staying well-hydrated and encouraging gentle movement prevent clot formation and promote healthy circulation.
Medical Interventions
- Anticoagulation Therapy: When thrombus formation is significant, blood thinners like warfarin or direct oral anticoagulants are prescribed, especially in deep vein thrombosis cases.
- Antibiotics: In cases where infection is the causal factor, targeted antibiotic therapy is essential.
- Vein Removal or Sclerotherapy: In recurrent or chronic cases, interventional procedures may be needed to eliminate or seal off problematic veins.
When to Seek Specialized Care
Persistent or worsening symptoms, signs of infection, or evidence of deep vein involvement require assessment by vascular medicine specialists. These professionals conduct appropriate diagnostics such as duplex ultrasound imaging to determine the extent of vein involvement and recommend personalized treatment plans.
Preventing Phlebitis: Lifestyle and Medical Strategies
Prevention is always preferable to treatment, especially with vascular health. Here are essential strategies:
- Maintain Physical Activity: Regular movement keeps blood flowing, reducing stasis and clot risk.
- Avoid Prolonged Immobilization: Take periodic breaks during long flights or sedentary work to stretch and walk around.
- Manage Underlying Conditions: Control autoimmune diseases and clotting disorders with medical supervision.
- Use Proper Medical Devices: Ensure IV lines are inserted and maintained by trained healthcare professionals.
- Healthy Lifestyle Choices: A balanced diet, weight management, and smoking cessation contribute significantly to vascular health.
The Role of Vascular Medicine in Managing Phlebitis
Specialists in vascular medicine, such as those you find at trufflesveinspecialists.com, possess the expertise to accurately diagnose phlebitis causes and treatment. Through advanced diagnostic tools and personalized treatment plans, vascular specialists aim to restore vein health, prevent recurrence, and minimize the potential for severe complications like pulmonary embolism or tissue damage.
Advancements in Phlebitis Management and Future Perspectives
The field of vascular medicine continually evolves, incorporating innovative techniques such as endovenous laser therapy, radiofrequency ablation, and targeted pharmacotherapy to treat venous inflammation more effectively. Researchers are also investigating the genetic and molecular mechanisms underpinning venous diseases to develop preventative strategies.
Conclusion: Empowering Vascular Health Through Knowledge and Care
Understanding the causes of phlebitis and the broad spectrum of treatment options empowers individuals to take proactive steps in maintaining their vascular health. Early diagnosis, appropriate medical intervention, and lifestyle modifications can significantly reduce the risk of complications, improving quality of life.
At Truffles Vein Specialists, we are committed to providing expert care in vascular medicine to help you manage and prevent venous conditions effectively. Prioritize your vein health today—consult with our specialists for personalized evaluation and treatment options tailored specifically to your needs.